对象与方法
一、研究对象
二、研究方法
三、手术方法
结果
一、一般资料
表1 11例腹盆腔复杂肿瘤患者一般资料 |
| 病 例 | 性别 | 年龄(岁) | 身高(cm) | 体质量(kg) | ICU住院时间(h) | 肿瘤情况 |
|---|---|---|---|---|---|---|
| 患者1 | 男 | 52 | 180 | 85 | 0 | 直肠癌术后转移 |
| 患者2 | 男 | 61 | 166 | 64 | 58 | 肾盂癌并癌栓、淋巴结转移 |
| 患者3 | 男 | 33 | 172 | 79 | 517 | 直肠癌术后转移 |
| 患者4 | 女 | 67 | 150 | 52 | 42 | 输尿管癌并淋巴结转移 |
| 患者5 | 女 | 44 | 156 | 56 | 108 | 宫颈癌术后转移 |
| 患者6 | 女 | 55 | 152 | 51 | 0 | 腹膜后平滑肌肉瘤 |
| 患者7 | 男 | 55 | 170 | 66 | 11 | 肾盂癌并淋巴结转移 |
| 患者8 | 女 | 52 | 157 | 48 | 0 | 肾盂癌术后种植 |
| 患者9 | 男 | 54 | 168 | 63 | 0 | 肾盂癌并癌栓、淋巴结转移 |
| 患者10 | 女 | 31 | 165 | 61 | 0 | 肠癌术后转移 |
| 患者11 | 男 | 65 | 168 | 55 | 0 | 膀胱癌 |
二、术中情况
表2 11例腹盆腔复杂肿瘤患者术中血管切除、手术时间及输血情况 |
| 病 例 | 术中血管切除情况 | 手术时间(min) | 输血种类及量 |
|---|---|---|---|
| 患者1 | 右侧髂外静脉节段性切除+右侧髂内动静脉节段性切除 | 570 | 4单位红细胞,150 ml血浆 |
| 患者2 | 下腔静脉节段性切除 | 900 | 4单位红细胞,1000 ml血浆 |
| 患者3 | 右侧髂内动静脉节段性切除+左侧髂外静脉节段性切除 | 780 | 30.5单位红细胞,5单位血小板,3600 ml血浆 |
| 患者4 | 下腔静脉节段性切除+双侧髂总静脉节段性切除+右侧 髂总动脉与髂外动脉人工血管搭桥术 | 570 | 6单位红细胞,1800 ml血浆 |
| 患者5 | 下腔静脉节段性切除+右侧髂外动脉静脉节段性切除+ 右侧髂外动脉人工血管置换 | 750 | 9.5单位红细胞,600 ml血浆 |
| 患者6 | 下腔静脉节断性切除 | 420 | 2单位红细胞,200 ml血浆 |
| 患者7 | 下腔静脉节段性切除 | 420 | 2单位红细胞,600 ml血浆 |
| 患者8 | 右侧髂外静脉节段性切除 | 500 | 1.5单位红细胞 |
| 患者9 | 下腔静脉节段性切除 | 675 | 15单位红细胞,1200 ml血浆,10单位冷沉淀 |
| 患者10 | 下腔静脉节段性切除 | 390 | 无 |
| 患者11 | 左侧髂外静脉节段性切除 | 630 | 无 |
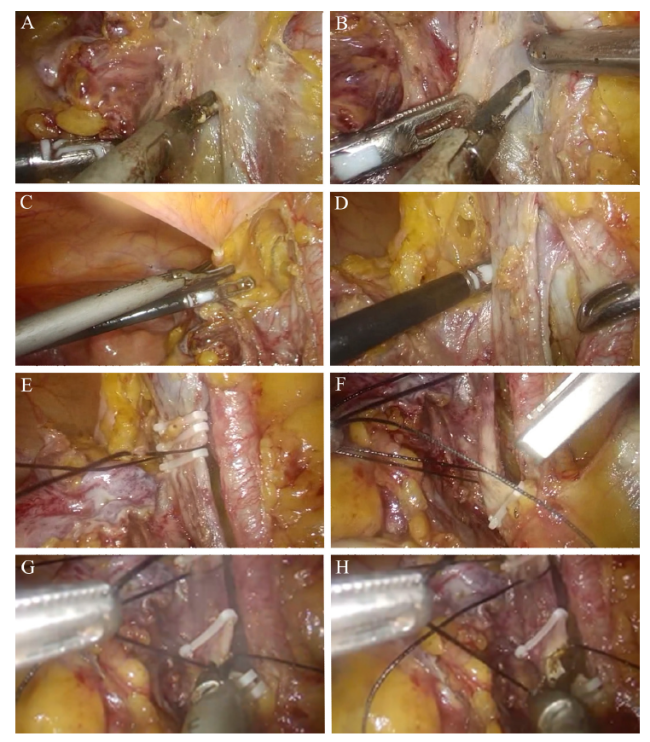
图1 下腔静脉节段性切除手术过程A:游离髂外静脉下缘;B:建立髂外动静脉之间平面;C:结扎并离断脐内侧韧带;D:游离远端髂外静脉下缘;E:结扎髂外静脉远端;F:结扎髂外静脉近端;G、H:节段性切除下腔静脉 |
表3 11例腹盆腔复杂肿瘤患者下肢血栓及血管评估相关情况 |
| 病 例 | 下肢血栓情况 | 术前CT/MRI了解血管情况 | 下肢侧支循环 |
|---|---|---|---|
| 患者1 | 术后右侧髂外静脉远心段、股总静脉、股静脉近段、股深静脉近段、小腿肌间静脉血栓 | 肿瘤压迫、粘连右髂内、外动静脉 | 可能未建立 |
| 患者2 | 双下肢静脉血流通畅,未见血栓 | 肿瘤包绕、压迫下腔静脉 | 可能已建立 |
| 患者3 | 术后下肢静脉急性血栓形成(右侧肌间静脉、左侧股总静脉、左侧腘静脉、左侧胫后静脉其中1支、左侧腓静脉完全闭塞,左侧股静脉不完全闭塞) | 肿瘤侵犯左髂外静脉可能 | 可能未建立 |
| 患者4 | 术后第3日彩超未见血栓。术后第4周经彩超发现血栓:右侧股总静脉血栓形成(不完全闭塞) | 肿瘤包绕、压迫右髂外静脉 | 可能已建立 |
| 患者5 | 术后右下肢大隐静脉血栓后改变(部分再通), 术前已有血栓 | 肿瘤包绕下腔静脉、右髂外动静脉 | 可能已建立 |
| 患者6 | 出院后未继续服用抗凝药物,术后1月余因下肢水肿发现下肢静脉血栓(髂静脉远心端及股总静脉、股深静脉、胫前、胫后静脉及部分肌间静脉闭塞),水肿难以消退、予以介入溶栓治疗 | 肿瘤包绕并累及下腔静脉 | 可能已建立 |
| 患者7 | 双侧下肢静脉血流缓慢,未见血栓 | 局段性压迫下腔静脉 | 可能未建立 |
| 患者8 | 双下肢静脉血流通畅,未见血栓 | 肿瘤局部压迫、粘连右髂外静脉 | 可能未建立 |
| 患者9 | 双下肢静脉血流通畅,未见血栓 | 癌栓几乎完全堵塞下腔静脉 | 可能已建立 |
| 患者10 | 双下肢静脉血流通畅,未见血栓 | 肿瘤包绕下腔静脉 | 可能已建立 |
| 患者11 | 左侧下肢静脉急性血栓形成(左髂外静脉至左侧股总静脉静脉完全闭塞) | 肿瘤压迫、粘连左髂外静脉 | 可能未建立 |