组织学是部分ILD患者诊断中极其重要的一部分,临床上获取组织学标本的手段主要包括SLB、TBLC、TBFB和经皮肺穿刺活检等
[5]。SLB是被推荐最多的组织取材手段,可明显提高诊断准确率,但由于SLB与患者肺活检术后死亡率增加明显相关
[6],因此在临床上应用于ILD受限。近年来TBLC的临床价值逐步受到肯定。既往研究证明,TBLC在ILD方面的临床诊断率可与SLB相当
[6⇓-8]。Tomassetti等
[7]在2016年发表的回顾性队列研究共纳入117例受试者(58例TBLC、59例SLB),结果显示两者在ILD诊断方面比较差异无统计学意义。2019年COLDICE研究成果发表,此项前瞻性多中心队列研究共纳入65例ILD患者,全身麻醉下行TBLC和SLB,两者在病理诊断一致率高达70.8%,临床诊断一致率高达76.9%;同时,TBLC的出血风险约22%,以轻到中度出血为主,安全性较好
[8]。在此基础上,近年来的临床研究进一步探究了TBLC对于不同类型ILD患者的诊断效能。2019年Romagnoli等
[9]的一项小样本研究中(
n =21),TBLC诊断IPF比例最高(9/21)。2022年Zaizen等
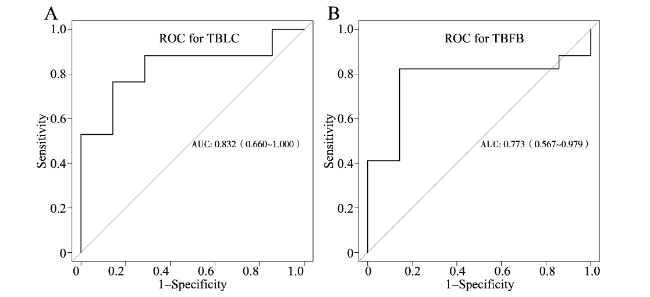
[10]对TBLC在ILD不同病因的诊断灵敏度方面进行更为细致的研究,结果显示TBLC诊断特发性间质性肺炎的灵敏度最高,其次是过敏性肺炎、结缔组织病相关性间质性肺病(如系统性硬化)。进一步研究发现,TBLC在特发性间质性肺炎中的诊断灵敏度高于非特异性间质性肺炎、过敏性肺泡炎和结缔组织病相关性间质性肺病。考虑到临床安全性和可行性,为进一步比较TBLC与TBFB在ILD诊断方面的价值,本研究于同一ILD患者病变处行TBFB和TBLC取材,减少影响因素,结果显示未发生严重出血事件。同时本研究结果也显示,TBLC对ILD的诊断率高于TBFB。这说明,TBLC在ILD患者诊断安全性可行的基础上,诊断效能较TBFB更可观。2022年欧洲呼吸学会(European Respiratory Society,ERS)指南中也明确提到TBLC对于无法明确病因的ILD有重要的诊断价值,推荐结合患者的临床特征、肺部高分辨率CT等方面综合判断,在多学科讨论的基础上做出最终病因的诊断
[11-12]。